In 2014 Californias personal health care spending was highest in the nation 2950 billion representing 115 percent of total US. ECM typically supports multiple users in a collaborative environment by integrating document management digital asset management and record retention.
 Share Is Prepared To Help Hospital Systems Comply With Cms Onc Final Interoperability Rule State Health Alliance For Records Exchange Share
Share Is Prepared To Help Hospital Systems Comply With Cms Onc Final Interoperability Rule State Health Alliance For Records Exchange Share
A content management system CMS is a computer software used to manage the creation and modification of digital content.
What is cms in healthcare. Medicaid another type of government health insurance program provides health coverage to low-income people as well as families and children pregnant women and others. What is a Quality Measure What is a Quality Measure. Comparing historical state rankings through 2014 California consistently had the highest level of total personal health care spending together with the highest total population in the nation.
Other large states New York. Darüber hinaus versteht sich CMS als Sparringspartner für. Practice Transformation is a process that results in observable and measurable changes to practice behavior.
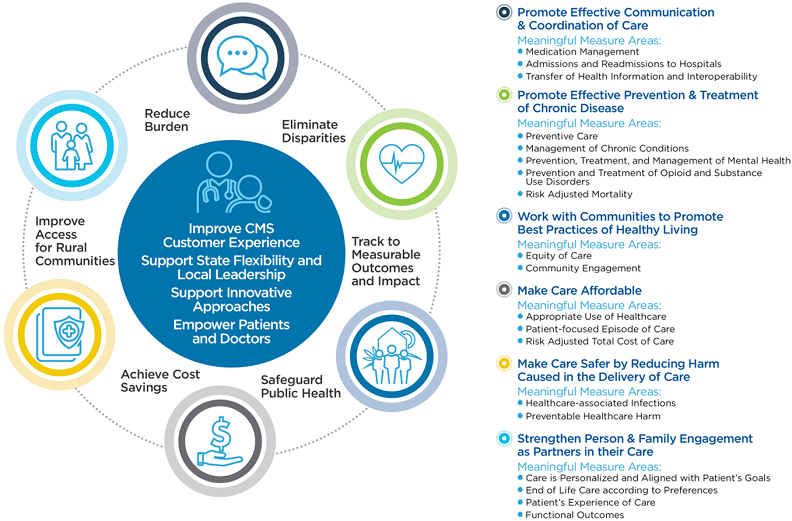
CMS Deutschland berät YEH strategisch und exklusiv in allen rechtlichen Fragen. Combined with the industrys most extensive network access to healthcare data Ciox Healths expertise relationships technology and scale make a difference for healthcare stakeholders and empower greater health for. The framework aims to improve outcomes for patients their families and health systems while also reducing burden on clinicians and providers.
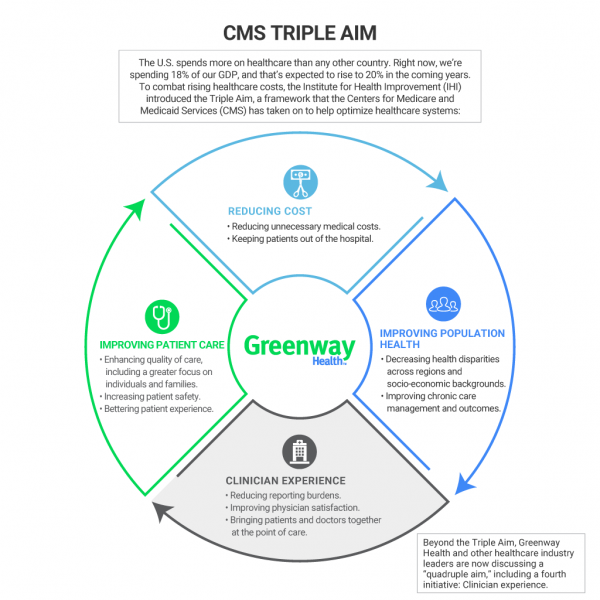
The Centers for Medicare Medicaid Services CMS today adopted new provisions to lower maximum out-of-pocket costs to consumers by 400 while increasing competition and improving the consumer experience for millions of Americans who will rely on the Federal Health Insurance Marketplaces in plan year 2022. Ciox Health a leading health technology company simply and securely connects healthcare decision makers with the data and hidden insights in patient medical records. The Center for Medicare Medicaid Services CMS seeks information about large scale transformation of clinician practices to accomplish our aims of better care and better health at lower costs.
As CMS develops clinical quality measures CMS cannot do it without making a sustained long-term commitment to take a holistic view. It is CMS responsibility to ensure that meaningful robust clinical quality measures CQMs are available for determination of quality and value of clinical care across all settings. Das Netzwerk Young Excellence in Healthcare YEH versteht sich als interdisziplinäres Bindeglied zwischen Young Professionals aus dem Gesundheitsmarkt und engagiert sich für intelligente Rahmenbedingungen der Gesundheitswelt von morgen.
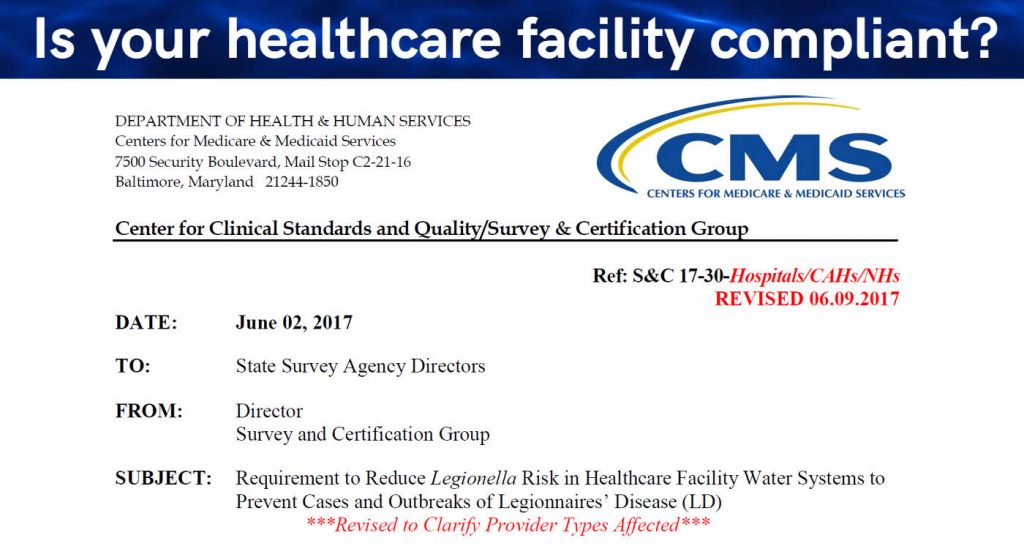
Quality measures are standards for measuring the performance of healthcare providers to care for patients and populations. This is called a defined-contribution plan. The CMS was concerned that the use of text messages in healthcare will lead to the exposure of sensitive patient data and could threaten the.
The Centers for Medicare Medicaid Services CMS is part of the. Ensuring data accuracy is critically important to both the Centers for Disease Control and Prevention CDC and the Centers for Medicare and Medicaid Services CMS for guiding prevention priorities and protecting patients. Personal health care spending.
Quality measures can identify important aspects of care like safety effectiveness timeliness and fairness. What is CMS meaning in Nursing. The CMS comprehensive Meaningful Measures initiative identifies high-priority areas for quality measurement and improvement.
Centers for Medicare Medicaid Services CMS The federal agency that runs the Medicare Medicaid and Childrens Health Insurance Programs and the federally facilitated Marketplace. In November the Centers for Medicare and Medicaid Services CMS explained in emails to healthcare providers that the use of text messages in healthcare is prohibited due to concerns about security and patient privacy. You could be eligible for both programs and Medicare and Medicaid are both administered by the Centers for Medicare Medicaid Services CMS.
CMSs are typically used for enterprise content management ECM and web content management WCM. Physicians and their care teams are the most vital resource a patient has. In health reimbursement agreements employers determine how much money to contribute to employees as compensation for their healthcare costs.
CMS All Acronyms viewed May 18 2021 CMSnursing. Centers for Medicare and Medicaid Services CMS explains how various healthcare reimbursement approaches and group health insurance plans affect employees and employers. SMS messages are not secure.
The Center for Medicare and Medicaid Innovation CMMI also known as the Innovation Center was authorized under the Affordable Care Act ACA and.
 Understanding Cms S Triple Aim Greenway Health
Understanding Cms S Triple Aim Greenway Health
 Cms Highlights Four Years Of Accomplishments In Healthcare Simpleltc
Cms Highlights Four Years Of Accomplishments In Healthcare Simpleltc
 Cms Centers For Medicare Medicaid Services Say Hello
Cms Centers For Medicare Medicaid Services Say Hello
 Cms Mandates Water Management Programs In Healthcare Facilities Vertex
Cms Mandates Water Management Programs In Healthcare Facilities Vertex
 Oneupweb Choosing The Right Cms For Healthcare Websites
Oneupweb Choosing The Right Cms For Healthcare Websites
 Centers For Medicare Medicaid Services Wikipedia
Centers For Medicare Medicaid Services Wikipedia
 April 26 2018 May 2 2018 Cms Quality Measures How They Are Used And How You Can Be Involved Youtube
April 26 2018 May 2 2018 Cms Quality Measures How They Are Used And How You Can Be Involved Youtube
 Cms Verma Talks Healthcare Regulations With Providers Fiercehealthcare
Cms Verma Talks Healthcare Regulations With Providers Fiercehealthcare
 Cms Quality Measures Promote Patient Centered Care
Cms Quality Measures Promote Patient Centered Care
 Cms Innovation Center Set To Launch Ai Health Outcomes Challenge Healthcare It News
Cms Innovation Center Set To Launch Ai Health Outcomes Challenge Healthcare It News
 Interoperability In Healthcare What The Proposed Onc Cms Rule Changes Mean
Interoperability In Healthcare What The Proposed Onc Cms Rule Changes Mean
 Choosing The Best Cms For A Healthcare Organization Or Hospital Centretek
Choosing The Best Cms For A Healthcare Organization Or Hospital Centretek
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.