Check that medications are covered. You can also see if each plan requires Prior Authorization Step Therapy or has Drug Quantity limit for Revlimid.
 The Out Of Pocket Cost Burden For Specialty Drugs In Medicare Part D In 2019 Findings 9278 Kff
The Out Of Pocket Cost Burden For Specialty Drugs In Medicare Part D In 2019 Findings 9278 Kff
You can also see if each plan requires Prior Authorization Step Therapy or has Drug Quantity limit for Revlimid.

Does medicare pay for revlimid. Please answer the following questions and fax this form to the number listed above. 2020 Medicare Drug Plan Cost for Revlimid. Treatment differed significantly based on the type of prescription drug coverage.
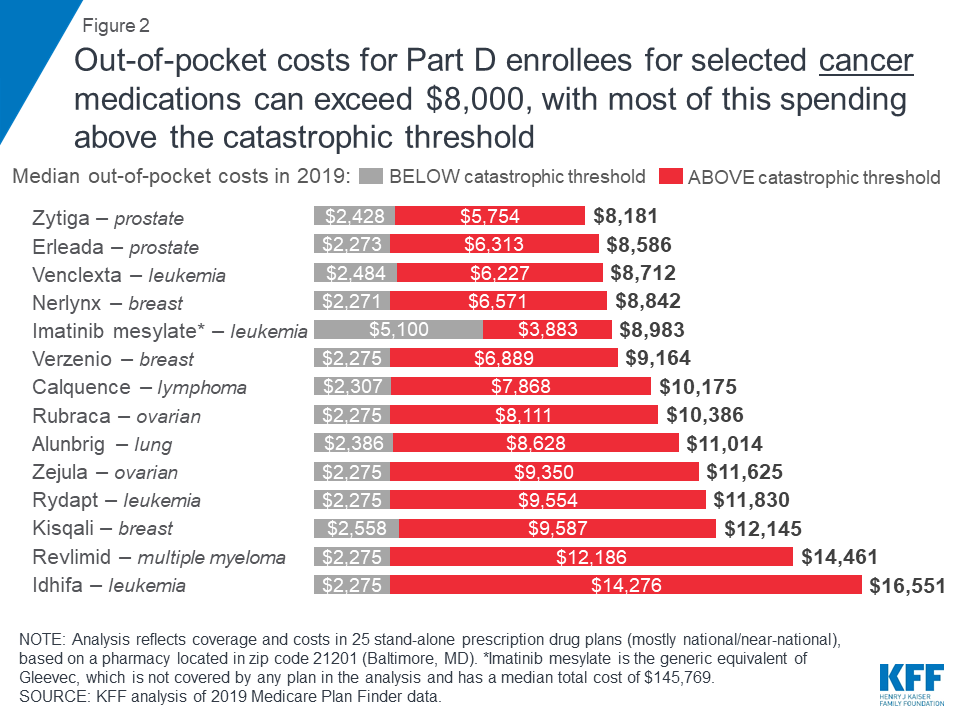
Certain requests for coverage require review with the prescribing physician. For example 84 percent of an enrollees out-of-pocket costs for Revlimid a drug to treat multiple myeloma would occur in the catastrophic phase which. Your doctor or other health care provider may recommend you get services more often than Medicare covers.
Celgene the manufacturer of Revlimid offers a program called. Fortunately for her taking a pill called Revlimid made by Celgene can hold the disease at bay. Since Revlimid is not on any formularly the insurance co.
If you need financial support to pay for Revlimid or if you need help understanding your insurance coverage help is available. Similarly Medicare also covers radiation therapy for cancer patients. But its cost began eating her up.
The chart includes the plans premium and deductible for every plan that offers additions coverage for Revlimid. The amount of the co-pay varies from company to company and plan to plan. Drug prescribing varied considerably among states KHN found.
Medicare patients or their caregivers should ensure that needed medications such as bortezomib Velcade lenalidomide Revlimid or thalidomide Thalomid. For two of the 10 drugs. Dispensed for 24637 patients Revlimid cost 8778 per claim.
PDP enrollees were also 38 less likely to receive classic cytotoxic agents. Medicare helps pay for an injectable drug if youre a woman with osteoporosis who meets the criteria for the Medicare home health benefit and has a bone fracture that a doctor certifies was related to post-menopausal osteoporosis. In the deductible phase beneficiaries are on their own and must pay the full retail price for their medications.
Revlimid - Medicare Phone. Probably has a co-pay associated with non-formularly drugs. Below is your cost or co-pay for Revlimid in Stanislaus County California.
For chemotherapy given in a doctors office or freestanding clinic you pay 20 of the Medicare-approved amount and the Part B Deductible applies. Medicare Part B generally covers outpatient chemotherapy cancer treatments such as in a freestanding clinic or doctors office. Between the deductible and initial coverage limit the insurer or.
Tier 5 drugs are usually non-preferred brand-name drugs. That totaled more than 13 billion. 866-371-3239 Health Partners Plans manages the pharmacy drug benefit for your patient.
Below is your cost or co-pay for Revlimid in Santa-Clara County California. Does Medicare cover Revlimid. Adjusting for baseline characteristics the study showed that compared to those with no coverage Medicare Part D enrollees were 6 more likely to receive active care and 14 less likely to receive parenteral care.
Revlimid is available as a brand name drug only a generic version is not yet available. A doctor must certify that you cant give yourself the injection or learn how to give yourself the drug by injection. 215-991-4300 Fax back to.
The cost for Revlimid oral capsule 25 mg is around 23317 for a supply of 28 capsules depending on the pharmacy you visit. A recent analysis by the Kaiser Family Foundation finds that Medicare recipients taking Revlimid for cancer could end up paying on average 11538 out of pocket for the drug in 2016 even if the. Medicare plans typically list Revlimid in Tier 5 of their formulary.
In this case youd pay 20 of the Medicare-approved amount after paying the Medicare Part B deductible. Rhode Island and Nebraska had the. Most Medicare Advantage beneficiaries 88 percent are enrolled in MA-PDs.
For these specialty tier drugs median annual out-of-pocket cost increases range from 224 for Copaxone a multiple sclerosis drug to 2923 for Revlimid a cancer drug. Please check the formulary for different brand and generic drug names. Please note any information left blank or illegible may delay the.
If your Rituxan treatment is covered by Medicare Part B you will typically be responsible for paying the Part B coinsurance or copayment 20 percent of the Medicare approved amount after you meet the Part B deductible which is 185 per year in 2019. Tier 5 drugs cost more than Tier 1 2 3 and 4 drugs. 100 of Medicare Advantage plans and Medicare Part D plans cover Revlimid.
Prices are for cash paying customers only and are not valid with insurance plans. BUT and this is a big BUT It is possible Revlimid will be covered under Medicare Part B if it is given to him by a technician in a docs office. Medicare Advantage plans that offer prescription drug coverage are called Medicare Advantage Prescription Drug Plans MA-PD.
If youre covered under Medicare Part A youll pay the inpatient deductible. The chart includes the plans premium and deductible for every plan that offers additions coverage for Revlimid. Does your plan have restrictions.
In January of 2017 Holt facing a monthly list price of 12837.